Diabetes is a chronic illness that affects how the body processes blood sugar (glucose). In people with diabetes, this process does not work properly, leading to increased levels of blood sugar in their bodies. Diabetes can be classified into two types: Type 1 and Type 2. There are differences between these two types in relation to causative factors, symptoms, treatments, and overall health effects.
WHAT IS TYPE 1 DIABETES?
Type 1 diabetes, which used to be called Juvenile-Onset or Insulin-Dependent Diabetes Mellitus (IDDM), is an autoimmune disease where the immune system erroneously attacks and destroys insulin-producing beta cells in the pancreas. This leads to inadequate insulin production or a complete lack of the hormone, hence preventing glucose from entering cells for energy, resulting in its buildup in the bloodstream.
CAUSES AND RISK FACTORS:
The underlying cause of Type 1 diabetes involves a combination of genetic and environmental factors. Unlike Type 2 diabetes, lifestyle choices such as diet do not play any role in developing Type 1 diabetes. It can also develop later on during adulthood, but most commonly, it starts during childhood.
SYMPTOMS:
Common early signs of Type 1 include:
- Unquenchable thirst and frequent urination
- Significant weight loss without trying
- Hunger pangs even after eating
- Tiredness and weakness
- Blurring eyesight
- Irritability coupled with mood swings
MANAGEMENT:
People living with Type 1 diabetes have to take insulin all their lives because there is no more production by the destroyed beta cells located in the pancreas. This can be achieved through daily injections or sustained infusion using an insulin pump. In addition, maintaining balanced diets and engaging in everyday physical exercises are key requirements needed for appropriately handling such conditions.
General Comparison of Type 1 vs. Type 2:
WHAT IS TYPE 2 DIABETES?
The most prevalent type of diabetes, Type 2 diabetes, accounts for about 90-95% of all diagnosed cases. In Type 2 diabetes, the main issue is either that the body cells become resistant to insulin or that the pancreas does not produce enough insulin to keep glucose within the normal range. Most intermediate adults are affected by this and can be prevented through proper lifestyle choices.
CAUSES AND RISK FACTORS:
The risk factors associated with Type 2 diabetes include poor eating habits, especially among those who consume sugary drinks and fail to engage in vigorous physical activities, leading to sedentary lifestyles. At the same time, obesity, especially when there is an increase in fat accumulation around one’s waist, also poses a great risk because it can result in insulin resistance, hence being diabetic.
SYMPTOMS:
Type 2 symptoms develop slowly over time, making them less noticeable than their counterparts in Type 1 diabetes. They may include:
- Extreme thirst and frequent urination
- Constant fatigue
- Unintentional weight loss
- Opaque sight
MANAGEMENT:
Managing Type 2 diabetes requires lifestyle changes, such as adopting good dieting habits and engaging in regular exercises. Such adjustments have been found possible to reverse the condition among some patients without medication use. However, depending on the severity of their conditions, oral medications or injectable therapies may be necessary for some patients, while others may not need any treatment at all apart from close monitoring by healthcare providers to avoid the negative effects of such drugs.
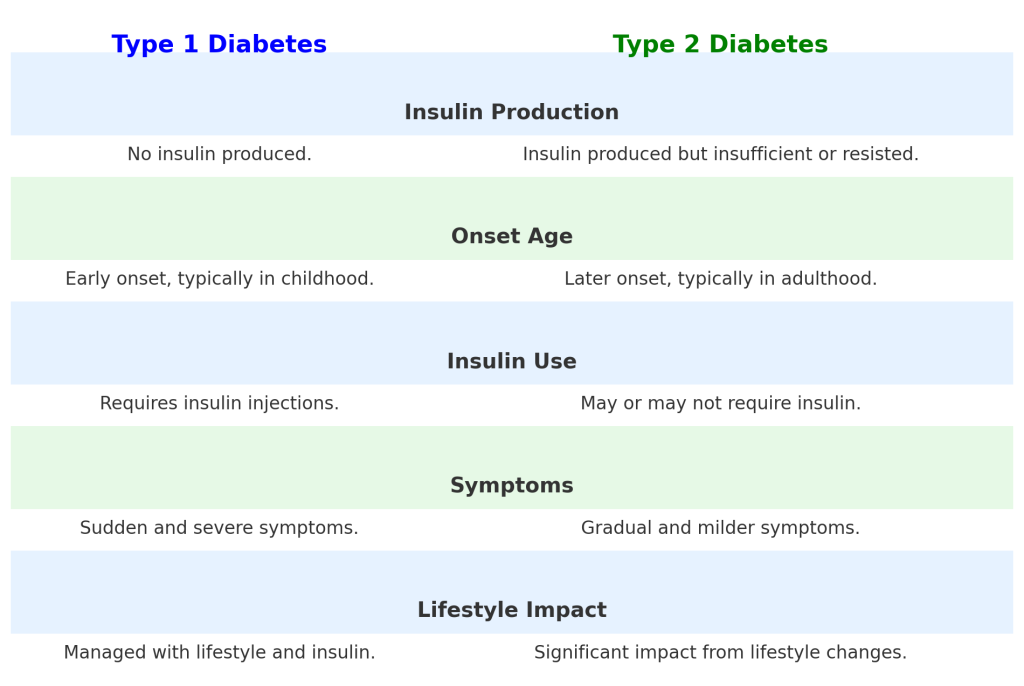
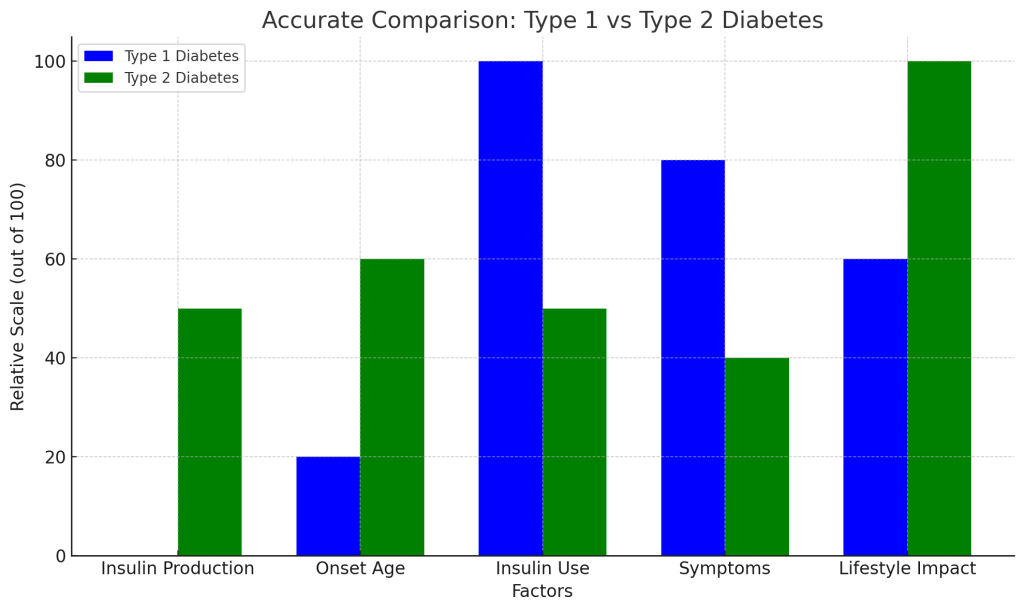
THE MAIN DISTINCTIONS BETWEEN TYPE 1 AND TYPE 2 DIABETES
Origin and Cause:
- Type 1: It occurs suddenly and usually during childhood or adolescence, caused by an immune attack on beta cells producing insulin.
- Type 2: This occurs gradually in adulthood, often influenced by environmental factors, including obesity and a sedentary lifestyle.
Insulin Production:
- Type 1: Small amounts of insulin are produced by the body.
- Type 2: The body becomes resistant to it or doesn’t produce enough of it.
Therapy:
- Type 1: Lifelong therapy with insulin is necessary.
- Type 2: Changes in lifestyle, medications taken orally, and sometimes insulin are sufficient for the treatment of Type 2 diabetes.
Prevalence:
- Type 1: Covers about ten percent of people suffering from diabetes.
- Type 2: About ninety-five percent of individuals living with diabetes are affected by this form of the disease.
Conclusion
However, both Type 1 and Type 2 diabetes require continuous care as they are serious diseases, but understanding their differences can help one manage them properly to avoid complications that arise from ignorance. Early detection is important because proper management is vital if one is to live a healthy life with diabetes without any health condition. With appropriate treatment, help from friends, relatives, or caretakers, and necessary adjustments in lifestyles, diabetics can still lead an active life, which will be satisfying enough for them.